Will Insurance Cover Wegovy

In recent years, Wegovy has gained significant attention as a weight management medication, offering a promising solution for individuals struggling with obesity. However, one of the crucial aspects potential users consider is whether their insurance plans cover this prescription drug. This article aims to provide an in-depth analysis of Wegovy's insurance coverage, shedding light on the various factors that determine accessibility and affordability for those seeking this treatment option.
Understanding Wegovy and its Mechanism of Action

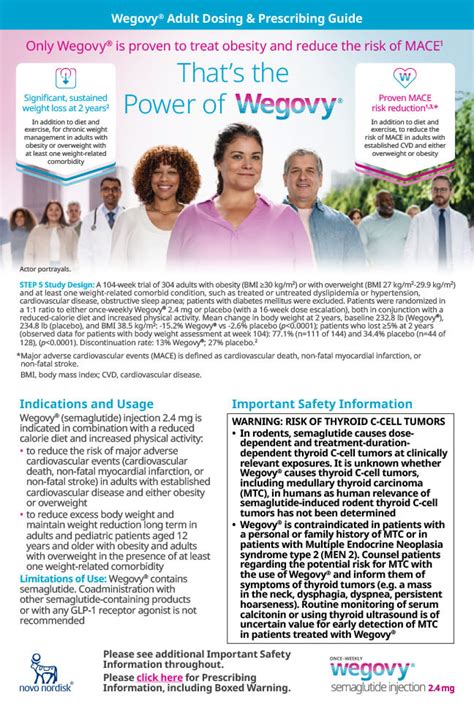
Before delving into the insurance coverage aspect, it’s essential to understand what Wegovy is and how it works. Wegovy, also known by its generic name Semaglutide, is a glucagon-like peptide-1 (GLP-1) receptor agonist. It belongs to a class of medications that help regulate blood sugar levels and promote weight loss. GLP-1 is a hormone naturally produced in the body, and Wegovy mimics its effects, leading to reduced appetite and increased feelings of fullness.
The medication is administered as a once-weekly injection, providing a sustained release of semaglutide into the body. This slow release mechanism ensures a steady effect, making it a convenient option for long-term weight management. The drug's effectiveness has been supported by numerous clinical trials, showing significant weight loss in obese individuals when combined with a healthy diet and exercise.
Insurance Coverage for Wegovy: An Overview
Insurance coverage for Wegovy can vary widely depending on several factors, including the insurance provider, the specific plan, and even the state or region in which the policyholder resides. While some insurance plans may cover Wegovy fully or partially, others might exclude it from their formulary, leaving the cost entirely to the patient.
The good news is that an increasing number of insurance providers are recognizing the importance of obesity treatment and the role of medications like Wegovy in managing this condition. Many plans now include Wegovy as a covered benefit, especially for individuals with obesity-related comorbidities such as type 2 diabetes, high blood pressure, or sleep apnea.
Factors Influencing Insurance Coverage
- Medical Necessity: Insurance companies often require a prior authorization process to determine if a medication is medically necessary for the patient. This involves the patient’s healthcare provider submitting detailed medical records and justifications for the prescription. Wegovy’s coverage is more likely to be approved if the patient has a body mass index (BMI) of 30 or higher, or a BMI of 27 or higher with one or more obesity-related conditions.
- Plan Formulary and Tier Placement: Insurance plans typically have a list of approved medications known as a formulary. The position of a drug on this list, often referred to as its tier, can impact coverage and cost. Some plans may place Wegovy in a higher tier, resulting in a higher out-of-pocket expense for the patient. However, many plans are moving towards placing obesity medications like Wegovy in lower tiers to encourage their use and improve patient access.
- Network and Provider Restrictions: Insurance coverage can also depend on the healthcare providers and facilities within the insurance network. If a patient seeks treatment or prescriptions from out-of-network providers, their insurance may not cover Wegovy or may cover it at a lower rate.
- Individual Plan Benefits: Different insurance plans offer varying levels of coverage. Some plans may have a comprehensive pharmacy benefit package that includes coverage for obesity medications, while others might have limited or no coverage for these drugs.
Analyzing Real-World Insurance Coverage Scenarios
To provide a more concrete understanding, let’s explore some real-world examples of insurance coverage for Wegovy:
Example 1: Commercial Insurance Plan
John, a 45-year-old individual with a BMI of 32 and high blood pressure, is enrolled in a commercial insurance plan through his employer. His plan includes coverage for obesity medications, and Wegovy is listed in its formulary. However, it is placed in a higher tier, resulting in a higher copay for John. With a prescription from his healthcare provider, John pays a copay of $150 per month for his Wegovy injections.
Example 2: Medicaid Coverage
Sarah, a 38-year-old with a BMI of 40 and type 2 diabetes, is enrolled in her state’s Medicaid program. Fortunately, many state Medicaid programs cover obesity medications, including Wegovy. Sarah’s medication is fully covered by her Medicaid plan, allowing her to access Wegovy without any out-of-pocket expense.
Example 3: Medicare Part D Plans
Robert, a 62-year-old retiree with a BMI of 35 and sleep apnea, is enrolled in a Medicare Part D prescription drug plan. While Medicare doesn’t cover all obesity medications, many Part D plans offer some level of coverage. Robert’s plan includes Wegovy in its formulary, but it is placed in a specialty tier, meaning he must pay a larger percentage of the drug’s cost. With a prior authorization from his healthcare provider, Robert pays 25% of the total cost of Wegovy, which is significantly lower than the full price.
| Insurance Scenario | Coverage Level | Out-of-Pocket Cost |
|---|---|---|
| Commercial Insurance Plan | Partial Coverage | $150/month copay |
| Medicaid | Full Coverage | No out-of-pocket expense |
| Medicare Part D | Partial Coverage | 25% of total cost |

The Impact of Insurance Coverage on Patient Access and Outcomes
Insurance coverage plays a pivotal role in determining the accessibility and affordability of medications like Wegovy. Here’s how it can influence patient access and outcomes:
Improved Access to Effective Treatment
When insurance plans cover obesity medications, it becomes more feasible for patients to access these treatments. The high cost of medications like Wegovy can be a significant barrier for many individuals. With insurance coverage, patients can afford the medication, leading to improved access to effective weight management options.
Enhanced Adherence and Long-Term Benefits
Coverage for Wegovy can encourage patients to adhere to their treatment plans. When patients face high out-of-pocket costs, they may be less likely to fill their prescriptions or follow through with the treatment. Insurance coverage can remove this financial barrier, leading to better adherence and, consequently, improved long-term health outcomes.
Addressing Health Disparities
Insurance coverage for obesity medications can help address health disparities. Obesity disproportionately affects certain populations, including individuals with lower incomes and certain racial or ethnic groups. By covering medications like Wegovy, insurance providers can ensure that these populations have equal access to effective weight management options, potentially reducing health disparities.
Navigating Insurance Coverage for Wegovy: Practical Tips

Here are some practical tips for individuals seeking insurance coverage for Wegovy:
- Review Your Insurance Plan: Carefully examine your insurance plan's details, including the formulary, tier placement, and any specific benefits related to obesity medications.
- Consult Your Healthcare Provider: Discuss your options with your healthcare provider. They can guide you through the process of obtaining prior authorization and provide necessary medical records to support your case.
- Explore Patient Assistance Programs: Many pharmaceutical companies offer patient assistance programs that provide financial support for medications. Wegovy's manufacturer, Novo Nordisk, offers a program called NovoCare that can help cover the cost of the medication for eligible patients.
- Consider Prescription Savings Cards: Prescription savings cards, offered by pharmacies or pharmaceutical companies, can provide discounts on medications. While they don't replace insurance coverage, they can reduce the out-of-pocket expense for Wegovy.
- Shop Around for Insurance Plans: If you're in the market for a new insurance plan, research and compare different options. Look for plans that offer comprehensive coverage for obesity medications and have Wegovy listed in their formulary.
The Future of Insurance Coverage for Obesity Medications
The landscape of insurance coverage for obesity medications, including Wegovy, is evolving. As the medical community recognizes the significance of obesity as a chronic condition and the role of medications in its management, more insurance providers are likely to include these drugs in their formularies. Advocacy efforts and changing attitudes towards obesity treatment are driving this shift.
Furthermore, the success stories of individuals who have achieved significant weight loss and improved health outcomes with medications like Wegovy are compelling arguments for their inclusion in insurance coverage. These real-world examples demonstrate the value of these medications in managing obesity and its related comorbidities.
Conclusion: Empowering Patients through Informed Decision-Making
Understanding the insurance coverage landscape for Wegovy is a crucial step for individuals considering this medication for weight management. By being informed about their insurance plan’s coverage, patients can make more confident decisions about their treatment options. While insurance coverage varies, the increasing recognition of obesity as a treatable condition offers hope for improved access to effective medications like Wegovy.
As the medical community continues to advocate for better insurance coverage for obesity medications, patients can take an active role in their health journey by staying informed, consulting with healthcare providers, and exploring available resources. With the right support and information, individuals can access the treatments they need to achieve their weight loss goals and improve their overall health and well-being.
How much does Wegovy cost without insurance coverage?
+The out-of-pocket cost for Wegovy without insurance coverage can be significant. The medication is typically priced at several hundred dollars per month. However, it’s important to note that the actual cost can vary depending on the pharmacy and any available discounts or patient assistance programs.
Are there any generic alternatives to Wegovy that might be more affordable?
+As of my last update in January 2023, there are no generic alternatives to Wegovy available in the market. However, keep in mind that the patent for Wegovy may expire in the future, which could lead to the emergence of generic versions that might be more affordable.
Can I negotiate with my insurance company to cover Wegovy if it’s not currently included in my plan?
+Yes, it’s possible to negotiate with your insurance company to advocate for the inclusion of Wegovy in your plan. This process typically involves providing detailed medical records and justifications for the medication’s necessity. While it may not always be successful, it’s worth exploring this option with the support of your healthcare provider.