Covid Vaccine Cost Without Insurance
The COVID-19 pandemic has brought unprecedented challenges to healthcare systems worldwide, and the development and distribution of vaccines have been crucial in the fight against the virus. One common concern among individuals, especially those without insurance coverage, is the cost associated with receiving the COVID-19 vaccine. In this article, we will delve into the intricacies of the COVID-19 vaccine's pricing, exploring how costs are determined, who bears the financial burden, and the measures in place to ensure equitable access to vaccination, even for those without insurance.
Understanding the Cost of COVID-19 Vaccines
The cost of the COVID-19 vaccine varies depending on several factors, including the specific vaccine manufacturer, distribution channels, and regional healthcare policies. Unlike traditional pharmaceutical products, the pricing of COVID-19 vaccines has been a subject of intense negotiation and collaboration between governments, vaccine developers, and healthcare providers.
Vaccine Development and Manufacturing Costs
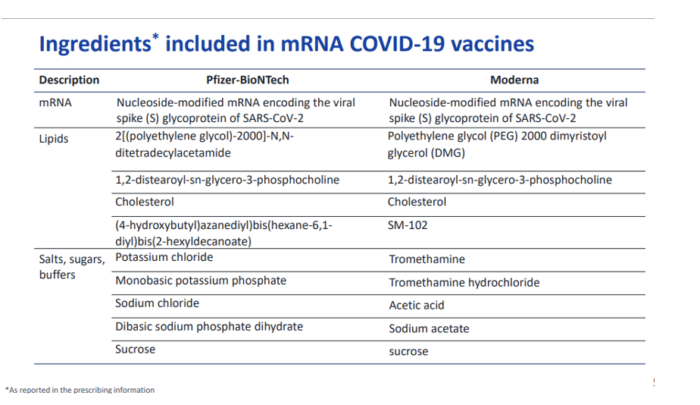
The development and manufacturing of COVID-19 vaccines have been rapid and innovative, with unprecedented global collaboration. However, these processes are incredibly expensive. Vaccine developers incur significant costs during research, clinical trials, and the scaling up of production facilities. The race to produce effective vaccines has led to substantial investments by pharmaceutical companies, governments, and international organizations.
For instance, Pfizer-BioNTech, one of the leading vaccine developers, has invested billions of dollars in research and development. Their vaccine, Comirnaty, is estimated to have cost approximately $25 billion to develop and produce, with a significant portion of these costs being recovered through sales and government subsidies.
Distribution and Administration Costs
Once vaccines are developed and manufactured, the next challenge is distributing them efficiently and equitably. This involves a complex logistics network, cold chain management, and administration by healthcare professionals. These distribution and administration costs can vary widely depending on the region and the healthcare infrastructure in place.
In the United States, for example, the Centers for Disease Control and Prevention (CDC) works closely with state and local health departments to coordinate vaccine distribution. The CDC provides funding and guidance to ensure that vaccines are allocated fairly and reach all communities. The cost of this distribution network is substantial and is often borne by a combination of federal, state, and local governments.
Pricing Strategies and Government Interventions
Vaccine pricing is a delicate balance between ensuring profitability for developers and making vaccines accessible to all. Governments and international organizations play a crucial role in negotiating prices and implementing policies to control costs.
In many countries, including the U.S., the government has negotiated bulk purchasing agreements with vaccine manufacturers. These agreements allow for a more stable and predictable supply of vaccines while also negotiating lower prices. For instance, the U.S. government secured a discounted price for the Pfizer-BioNTech vaccine through the Operation Warp Speed initiative.
Additionally, governments often provide subsidies or reimbursements to healthcare providers to cover the costs of vaccine administration. This ensures that even individuals without insurance coverage can access the vaccine without facing financial barriers.
COVID-19 Vaccine Pricing: A Global Perspective
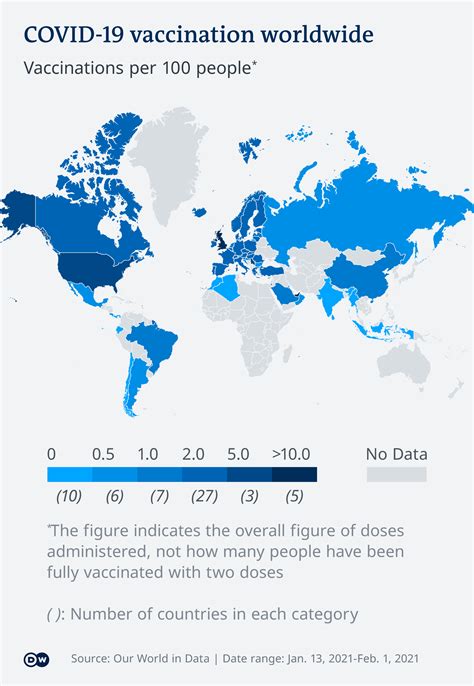
The cost of COVID-19 vaccines varies significantly across different regions and countries. While some countries have negotiated lower prices or received vaccines through international aid programs, others face higher costs due to their purchasing power or the absence of government subsidies.
Vaccine Pricing in the United States
In the United States, the cost of COVID-19 vaccines is primarily borne by the government and insurance providers. The CDC has implemented a policy that ensures individuals do not have to pay out of pocket for the vaccine itself. This means that even those without insurance are entitled to receive the vaccine at no cost.
However, there may be administrative fees associated with vaccine administration, especially at private healthcare facilities. These fees are typically covered by insurance providers, but for those without insurance, these costs can vary. According to the Health Resources and Services Administration (HRSA), individuals without insurance can expect to pay around $40 for vaccine administration fees.
International Vaccine Pricing
Internationally, vaccine pricing varies widely. Some countries have negotiated extremely low prices for vaccines, while others face higher costs. For instance, the European Union has secured relatively low prices for vaccines, with the Pfizer-BioNTech vaccine costing around €15.50 per dose. In contrast, developing countries may face higher costs due to limited negotiating power and infrastructure challenges.
Initiatives like COVAX, a global partnership aimed at equitable vaccine distribution, have been crucial in ensuring that lower-income countries can access vaccines at affordable prices. COVAX has secured vaccines for over 90 lower-income countries, ensuring that financial barriers do not hinder global vaccination efforts.
Ensuring Equitable Access for All
Despite the complexities of vaccine pricing, governments and international organizations have taken significant steps to ensure that COVID-19 vaccines are accessible to all, regardless of insurance status or financial means.
No-Cost Vaccination Programs
Many countries, including the United States, have implemented no-cost vaccination programs. This means that individuals, regardless of their insurance status, can receive the vaccine without any financial burden. These programs are often funded through government subsidies and are a crucial aspect of public health initiatives to control the pandemic.
In the U.S., the COVID-19 Public Health Emergency (PHE) Declaration has been instrumental in ensuring no-cost access to vaccines. Under this declaration, healthcare providers are prohibited from charging patients for the vaccine itself, although they may bill insurance companies or the HRSA for administrative fees.
Community Outreach and Vaccine Equity
To ensure equitable access, governments and healthcare organizations have implemented community outreach programs. These initiatives aim to reach underserved communities, provide education about vaccines, and address any barriers to access. Mobile vaccination clinics, community health workers, and cultural competency training are some strategies employed to ensure that no one is left behind in the vaccination drive.
Addressing Vaccine Hesitancy
Beyond financial barriers, vaccine hesitancy is another challenge that governments and healthcare providers must address. Misinformation and concerns about vaccine safety can deter individuals from getting vaccinated. To combat this, public health campaigns focus on providing accurate information, addressing concerns, and building trust within communities.
For instance, the CDC has developed comprehensive resources and educational materials to address vaccine hesitancy. These resources are available in multiple languages and formats, ensuring that information reaches diverse populations.
Future Implications and Conclusion
The COVID-19 pandemic has highlighted the importance of global collaboration and equitable access to healthcare. The development and distribution of vaccines have been pivotal in controlling the spread of the virus and saving lives. As we continue to navigate the pandemic, the lessons learned from vaccine pricing and accessibility will shape future public health strategies.
Moving forward, it is essential to maintain a balance between ensuring profitability for vaccine developers and making vaccines accessible to all. Governments and international organizations must continue to negotiate fair prices, provide subsidies where needed, and prioritize community outreach to address any barriers to vaccination.
The COVID-19 vaccine pricing landscape is complex, but with careful planning and collaboration, we can ensure that financial barriers do not prevent anyone from accessing life-saving vaccines. As we look towards a post-pandemic future, the lessons learned from this global health crisis will undoubtedly shape a more resilient and equitable healthcare system.
Frequently Asked Questions
Are COVID-19 vaccines free for everyone, regardless of insurance status?
+Yes, in many countries, including the United States, COVID-19 vaccines are free for all individuals, regardless of their insurance status. The vaccine itself is provided at no cost to the recipient, although there may be administrative fees associated with vaccine administration, which are typically covered by insurance or government subsidies.
How do governments negotiate lower vaccine prices?
+Governments negotiate lower vaccine prices through bulk purchasing agreements with vaccine manufacturers. These agreements allow governments to secure a more stable supply of vaccines and often result in discounted prices. International organizations like COVAX also play a crucial role in negotiating prices for lower-income countries.
What happens if I cannot afford the administrative fees for vaccine administration?
+In many cases, administrative fees for vaccine administration are waived for individuals who cannot afford them. Governments and healthcare providers often have programs in place to ensure that financial barriers do not prevent access to vaccination. You can contact your local health department or a community health center for more information on assistance programs.
Are there any ongoing efforts to reduce vaccine costs further?
+Yes, there are continuous efforts to reduce vaccine costs and improve accessibility. Governments, vaccine manufacturers, and international organizations are working together to streamline production processes, reduce development costs, and negotiate more favorable pricing. Additionally, initiatives like COVAX aim to ensure equitable access to vaccines globally, regardless of a country’s purchasing power.