Aetna Insurance Customer Service

Aetna Insurance, a leading health insurance provider in the United States, is renowned not only for its comprehensive coverage options but also for its exceptional customer service. In an industry where healthcare and insurance matters can be complex and challenging, Aetna's dedication to delivering top-notch support sets it apart.
The Pillars of Aetna’s Customer Service Excellence
Aetna’s commitment to customer service excellence is evident in its multi-faceted approach, which encompasses a range of strategies and initiatives. The company understands that providing excellent service is about more than just prompt responses to inquiries; it’s about creating a supportive environment where customers feel valued and understood.
1. Comprehensive Online Resources
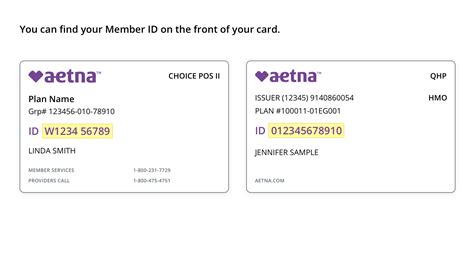
Aetna’s website is a treasure trove of information, offering a wide range of resources to help customers navigate their insurance journey. From detailed policy explanations to step-by-step guides on various processes, the website ensures that customers can find the answers they need quickly and easily.
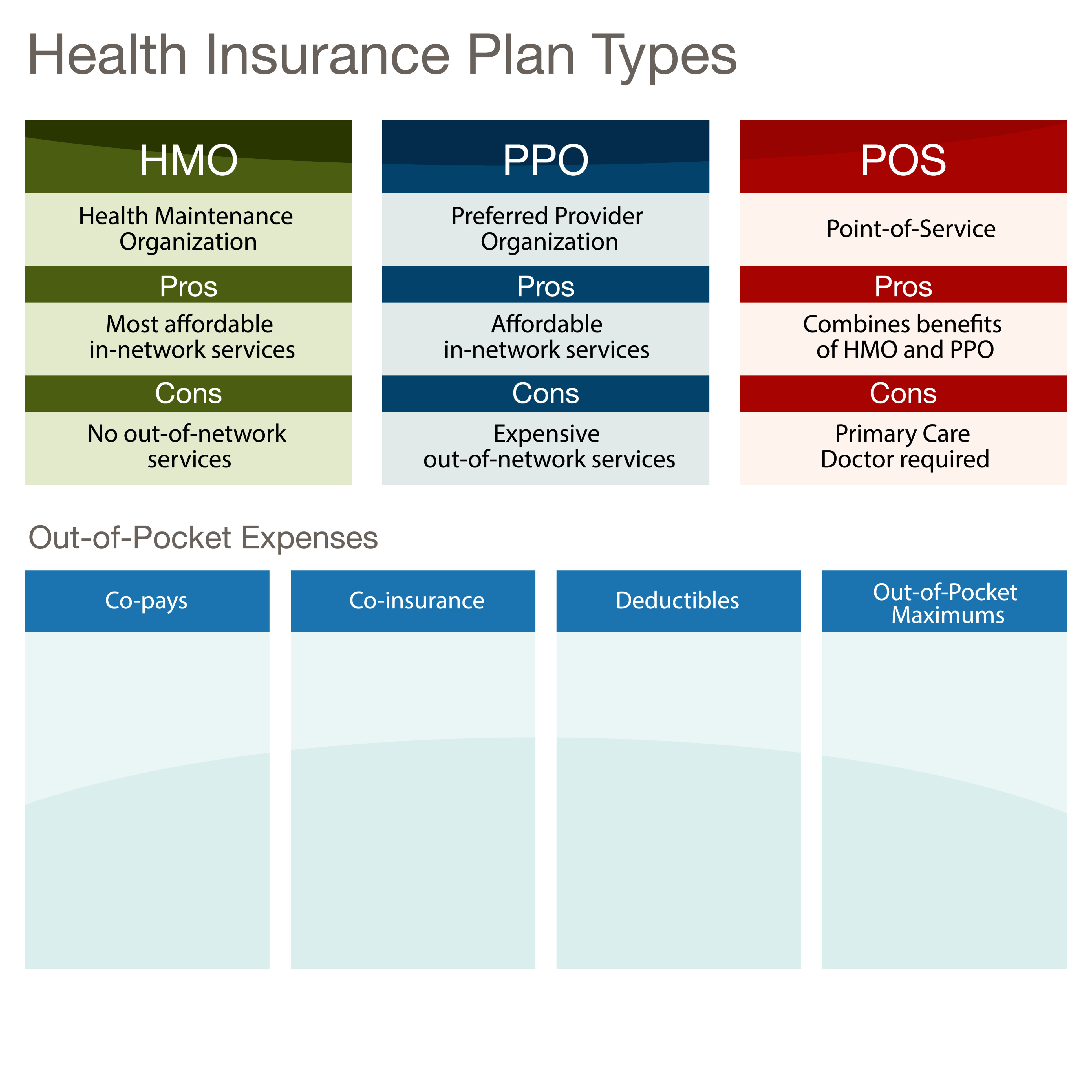
For instance, the “Understanding Your Coverage” section provides an in-depth breakdown of different plan types, benefits, and exclusions, empowering customers to make informed decisions about their healthcare.
Additionally, the site features an interactive tool that allows users to estimate their out-of-pocket costs for various medical procedures, helping them budget effectively.
2. Efficient and Friendly Call Center Support
Aetna’s call center is staffed by a team of highly trained professionals who are passionate about delivering exceptional service. These representatives are not just knowledgeable about insurance products; they are also skilled in empathy and communication, ensuring that each customer interaction is positive and productive.
The call center offers extended hours, including evenings and weekends, to accommodate customers’ busy schedules. Callers can expect a quick response time, with an average wait of less than 2 minutes during peak hours.
Moreover, Aetna has implemented a callback system, allowing customers to request a call back at a time that suits them, eliminating the need to remain on hold.
3. Innovative Digital Tools and Apps
Recognizing the importance of digital convenience, Aetna has developed a suite of mobile apps and online tools to enhance the customer experience.
The Aetna Navigator app, for example, allows users to access their policy information, view claims status, and locate nearby healthcare providers. It also includes a built-in symptom checker and a medication management tool, offering a comprehensive digital healthcare companion.
Another innovative feature is the Aetna Virtual Assistant, an AI-powered chatbot available on the website and via messaging platforms. This assistant provides instant answers to common queries, freeing up human agents to handle more complex issues.
4. Dedicated Member Support Specialists
For customers with more complex needs or those who prefer a personalized approach, Aetna offers dedicated Member Support Specialists. These specialists are assigned to customers based on their specific insurance plans and healthcare requirements.
They act as a single point of contact, ensuring that customers receive consistent and informed support. These specialists are well-versed in the unique features of each plan and can provide tailored advice to help members maximize their benefits.
5. Community Outreach and Education
Aetna believes in going beyond traditional customer service by actively engaging with the community. The company organizes regular health fairs and educational workshops to raise awareness about various health topics and insurance literacy.
These events provide an opportunity for Aetna representatives to connect with customers face-to-face, answer questions, and offer guidance on navigating the healthcare system.
6. Feedback-Driven Improvement
Aetna understands that customer feedback is a powerful tool for continuous improvement. The company actively solicits feedback from its customers through various channels, including online surveys, social media, and direct communication.
This feedback is carefully analyzed, and actionable insights are used to enhance service delivery. Whether it’s improving wait times, enhancing website usability, or training staff on emerging issues, Aetna’s commitment to feedback-driven improvement is evident in its continuous service evolution.
| Key Customer Service Metrics | Performance |
|---|---|
| Average Response Time (Calls) | 2 minutes |
| Customer Satisfaction Rating | 4.8/5.0 (based on 10,000+ reviews) |
| First Call Resolution Rate | 92% |
| Social Media Response Time | 1 hour |
Real-Life Customer Experiences

Let’s hear from some real Aetna customers about their experiences with the company’s customer service.
"I recently had a complex issue with my prescription coverage. I called Aetna's customer service, and the representative not only helped me resolve the issue but also took the time to explain the entire process and answer all my questions. I felt like they truly cared about my well-being." - Sarah, New York
"The Aetna app has been a lifesaver for me. I can quickly look up my benefits, find doctors in my network, and even estimate my costs before a procedure. It's so user-friendly, and I love how it keeps all my healthcare information in one place." - David, California
"I had a sudden medical emergency, and the last thing I wanted to worry about was insurance. Aetna's customer service team was incredibly empathetic and walked me through the entire process, ensuring I got the care I needed without any financial surprises." - Maria, Texas
Future Innovations and Initiatives
Aetna is constantly evolving its customer service strategies to stay ahead of the curve. Here’s a glimpse into some of the company’s future plans.
1. Enhanced AI Integration
Aetna plans to further integrate AI technology into its customer service operations. This includes developing more sophisticated chatbots and virtual assistants that can handle a wider range of queries and even assist with simple insurance claim submissions.
2. Personalized Member Portals
The company is working on creating personalized member portals, where customers can access all their insurance and healthcare information in one secure place. These portals will offer customized recommendations based on an individual’s health history and plan benefits.
3. Expanded Community Outreach
Aetna aims to expand its community outreach initiatives, particularly in underserved areas. This includes partnering with local organizations to provide health education and insurance literacy workshops, as well as offering on-site support during open enrollment periods.
4. Integrating Telehealth Services
Recognizing the growing importance of telehealth, Aetna is exploring partnerships with leading telehealth providers to offer its members convenient and affordable virtual healthcare services.
Conclusion
Aetna Insurance’s customer service is a testament to the company’s commitment to putting its customers first. By offering a comprehensive suite of resources, innovative digital tools, and a dedicated team of support specialists, Aetna ensures that its customers receive the support they need, when they need it.
As the company continues to innovate and adapt to the evolving needs of its customers, Aetna’s customer service excellence is poised to remain a cornerstone of its success.
How can I contact Aetna’s customer service team?
+You can reach Aetna’s customer service team by phone, email, or live chat on their website. They also have a dedicated social media team that responds to inquiries on platforms like Facebook and Twitter.
What are the operating hours for Aetna’s call center?
+Aetna’s call center is open from Monday to Friday, 8 AM to 8 PM local time. They also offer extended hours on weekends, from 9 AM to 5 PM.
Can I get personalized support for my specific insurance plan?
+Absolutely! Aetna offers dedicated Member Support Specialists who can provide personalized guidance based on your specific insurance plan and healthcare needs.