The Health Insurance Portability And Accountability Act

The Health Insurance Portability and Accountability Act, widely known as HIPAA, is a cornerstone piece of legislation in the United States that has revolutionized the healthcare industry, especially when it comes to patient privacy and data protection. Enacted in 1996, HIPAA has had a profound impact on the way healthcare providers, insurers, and businesses handle sensitive health information. This comprehensive article will delve into the various aspects of HIPAA, exploring its history, key provisions, enforcement, and its significance in today's digital age.
Understanding HIPAA: A Historical Perspective

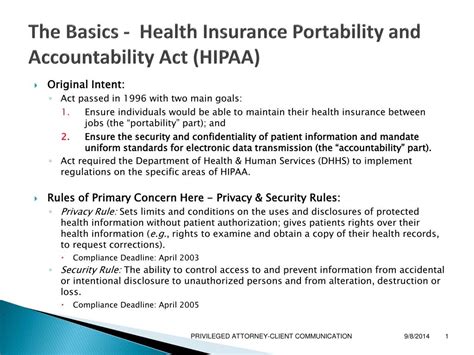
HIPAA was introduced during a time when the healthcare industry was undergoing significant changes. The act was designed to address two primary concerns: the need for individuals to maintain health insurance coverage, especially during periods of unemployment or career transitions, and the growing importance of safeguarding sensitive health data.
Prior to HIPAA, individuals faced numerous challenges when it came to health insurance. Gaps in coverage could lead to financial burdens and limited access to care. Additionally, the lack of standardized practices for handling health information resulted in potential privacy breaches and data misuse.
HIPAA aimed to rectify these issues by establishing a set of national standards to protect sensitive patient health information and ensure its confidentiality, integrity, and availability. It was a much-needed step towards building a more secure and efficient healthcare system.
Key Provisions of HIPAA
HIPAA is a comprehensive act that encompasses several crucial components. These include:
Health Insurance Portability
One of the initial objectives of HIPAA was to enhance health insurance portability. It aimed to ensure that individuals could retain their health coverage, even when changing jobs or experiencing other life events that might traditionally result in a loss of insurance. This provision was particularly beneficial for those with pre-existing medical conditions, as it prevented discrimination based on health status.
The Privacy Rule
The Privacy Rule, or the Standards for Privacy of Individually Identifiable Health Information, is a cornerstone of HIPAA. It sets forth national standards to protect individuals’ medical records and other personal health information. The rule provides patients with significant rights over their health information, including the right to access and receive a copy of their health records, the right to request corrections, and the right to be informed about how their health information is used and disclosed.
The Security Rule
Complementing the Privacy Rule is the Security Rule, which establishes a national set of security standards for protecting electronic protected health information (ePHI). This rule requires covered entities to implement administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of ePHI. It addresses issues like access control, audit controls, integrity controls, and transmission security.
Administrative Simplification
HIPAA’s Administrative Simplification provisions aim to streamline healthcare operations and improve efficiency. This includes standardizing electronic transactions, such as billing and payment processes, to reduce administrative burdens and costs. It also mandates the use of unique health identifiers for individuals, employers, health plans, and providers to facilitate data exchange.
Enforcement and Penalties
HIPAA includes provisions for enforcement and the imposition of penalties for non-compliance. The Department of Health and Human Services’ Office for Civil Rights (OCR) is responsible for enforcing HIPAA’s Privacy and Security Rules. Non-compliance can result in civil monetary penalties, with fines ranging from 100 to 50,000 per violation, up to a maximum of $1.5 million per year for violations of an identical provision.
HIPAA in the Digital Age
The advent of digital technology has transformed the healthcare landscape, and HIPAA has played a critical role in shaping how health information is handled in the digital realm. With the increasing use of electronic health records (EHRs) and the rise of telehealth services, HIPAA’s Security Rule has become even more vital in safeguarding patient data.
HIPAA-compliant practices ensure that patient data, whether stored or transmitted electronically, is protected against unauthorized access, use, disclosure, modification, or destruction. This includes implementing robust cybersecurity measures, encrypting data, and regularly training staff on data security protocols.
Telehealth and HIPAA Compliance
The COVID-19 pandemic accelerated the adoption of telehealth services, and HIPAA has been instrumental in guiding the secure delivery of remote healthcare. HIPAA permits the use of popular communication applications for telehealth services, provided that certain conditions are met. This includes ensuring the confidentiality of patient information and using encryption to protect data in transit.
Mobile Health Apps and HIPAA
The proliferation of mobile health (mHealth) apps has presented unique challenges for HIPAA compliance. While these apps offer numerous benefits, such as remote patient monitoring and improved access to healthcare, they also introduce new risks to patient privacy and data security. Developers and healthcare providers must ensure that any apps used for healthcare purposes are HIPAA-compliant.
Future Implications and Ongoing Challenges
As the healthcare industry continues to evolve, so too will the challenges and opportunities presented by HIPAA. The ongoing digital transformation of healthcare, the increasing use of artificial intelligence (AI) and machine learning, and the growing trend of precision medicine all present new frontiers for HIPAA compliance.
One of the key challenges is balancing the need for data sharing and collaboration in healthcare with the strict privacy and security requirements of HIPAA. Additionally, as cyber threats become more sophisticated, maintaining the security of patient data will remain a critical focus for healthcare providers and organizations.
The future of HIPAA will likely involve ongoing efforts to strike a delicate balance between enabling innovative healthcare solutions and maintaining the highest standards of patient privacy and data protection.
FAQ

What is the main purpose of HIPAA?
+The main purpose of HIPAA is to ensure the privacy and security of sensitive health information while also improving the portability and continuity of health insurance coverage.
Who does HIPAA apply to?
+HIPAA applies to covered entities, which include healthcare providers, health plans, and healthcare clearinghouses, as well as their business associates who handle protected health information (PHI) on their behalf.
What are the penalties for HIPAA violations?
+HIPAA violations can result in civil monetary penalties, with fines ranging from 100 to 50,000 per violation, up to a maximum of $1.5 million per year for violations of an identical provision. In some cases, criminal penalties may also apply.
How does HIPAA affect patient rights?
+HIPAA grants patients significant rights over their health information, including the right to access and receive a copy of their health records, the right to request corrections, and the right to be informed about how their health information is used and disclosed.
Can HIPAA-covered entities share patient information without consent?
+HIPAA allows covered entities to share patient information without consent for treatment, payment, and healthcare operations. However, for other purposes, such as marketing or research, patient authorization is generally required.