Health Insurance Portability And Accountability Act Of 1996

The Health Insurance Portability and Accountability Act (HIPAA) of 1996 is a landmark legislation in the United States that has significantly shaped the healthcare industry and the privacy and security of patient health information. Enacted on August 21, 1996, HIPAA aims to improve the efficiency and effectiveness of the healthcare system, protect health insurance coverage for workers and their families when they change or lose their jobs, and establish national standards to protect sensitive patient data. This comprehensive act has had a profound impact on healthcare providers, insurance companies, and individuals, ensuring the confidentiality, integrity, and availability of health information.
Understanding HIPAA: Key Provisions and Impact
HIPAA is a multifaceted law with several key provisions that address various aspects of the healthcare industry. One of its primary goals is to enhance the portability of health insurance, allowing individuals to maintain their coverage even when they change jobs or face certain life events. This provision aims to reduce the financial burden on individuals and promote continuity of care.
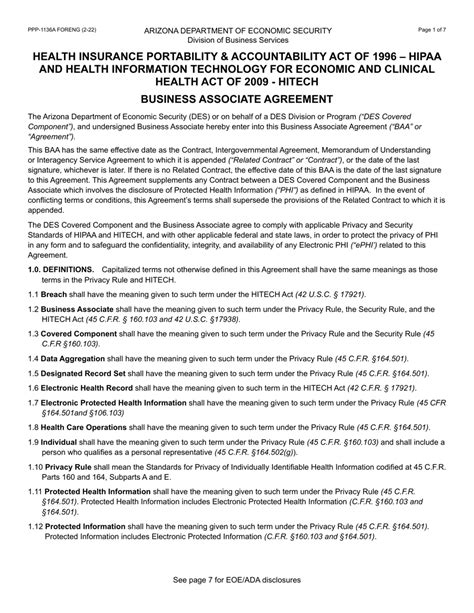
However, HIPAA is perhaps best known for its focus on privacy and security. The act establishes national standards for the protection of protected health information (PHI), which includes any individually identifiable health information, whether it is created, used, or disclosed in electronic, paper, or oral form. PHI covers a wide range of data, from names and addresses to medical records and payment information.
To safeguard PHI, HIPAA introduces a set of administrative, physical, and technical safeguards. These measures ensure that healthcare providers and their business associates implement appropriate security measures to protect patient data. Failure to comply with these standards can result in severe penalties, including fines and legal actions.
HIPAA Privacy Rule
The HIPAA Privacy Rule, or the Standards for Privacy of Individually Identifiable Health Information, is a critical component of the act. It outlines the rights of individuals regarding their health information and the obligations of covered entities to protect this information. The Privacy Rule grants patients the right to access their health records, request corrections, and receive a notice of privacy practices from their healthcare providers.
Covered entities, such as healthcare providers, health plans, and healthcare clearinghouses, must obtain patient consent before using or disclosing their PHI, except for specific purposes like treatment, payment, or healthcare operations. The Privacy Rule also sets limits on the use and disclosure of PHI, ensuring that patient information is handled with the utmost confidentiality.
HIPAA Security Rule
Complementing the Privacy Rule is the HIPAA Security Rule, which focuses on the protection of electronic PHI (ePHI). This rule requires covered entities to implement administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of ePHI. It addresses issues such as access control, encryption, audit controls, and contingency planning to safeguard patient data in the digital realm.
The Security Rule recognizes that the security of ePHI is an ongoing process and encourages covered entities to adopt a risk-based approach to security. This means regularly assessing potential threats and vulnerabilities and implementing appropriate measures to mitigate these risks.
HIPAA Breach Notification Rule
In 2009, the Breach Notification Rule was added to HIPAA to address the growing concern over data breaches. This rule requires covered entities and their business associates to notify affected individuals, the Department of Health and Human Services (HHS), and, in some cases, the media, following a breach of unsecured PHI. The notification process ensures that individuals are aware of any potential risks to their health information and can take appropriate action to protect their identities and well-being.
HIPAA Compliance and Enforcement
Ensuring HIPAA compliance is a critical responsibility for covered entities and business associates. The Office for Civil Rights (OCR), within the HHS, is responsible for enforcing HIPAA rules and investigating complaints. OCR can impose civil monetary penalties for non-compliance, with fines ranging from 100 to 50,000 per violation, with a maximum penalty of $1.5 million per year for repeat violations.
OCR investigates complaints, conducts audits, and takes corrective actions to ensure that covered entities are meeting their HIPAA obligations. In addition, the Department of Justice (DOJ) has the authority to prosecute cases of willful neglect or misuse of PHI, which can result in criminal penalties and significant fines.
Common HIPAA Violations
While the HIPAA regulations are comprehensive, some common violations can lead to non-compliance and potential penalties. These include failing to conduct regular risk assessments, inadequate training of workforce members, improper disposal of PHI, unauthorized access to PHI, and lack of proper security measures for ePHI.
To avoid these pitfalls, covered entities must stay updated with HIPAA guidelines, conduct regular audits, and invest in comprehensive training programs for their staff. Additionally, adopting robust security measures, such as encryption, access controls, and regular backups, is essential to safeguard PHI and maintain compliance.
HIPAA’s Impact on the Healthcare Industry
The implementation of HIPAA has had a profound effect on the healthcare industry, leading to significant changes in how patient data is handled and protected. Healthcare providers, insurers, and other covered entities have had to adapt their practices to meet the rigorous standards set by the act.
One of the most noticeable impacts of HIPAA is the increased focus on patient privacy and data security. Healthcare organizations now prioritize the protection of PHI, recognizing the potential consequences of data breaches and the importance of maintaining patient trust. This shift has led to the development of robust security measures and the adoption of cutting-edge technologies to safeguard patient information.
HIPAA and Healthcare Technology
The rise of electronic health records (EHRs) and health information technology (HIT) has presented both challenges and opportunities for HIPAA compliance. While EHRs and HIT systems offer improved efficiency and accessibility of patient data, they also introduce new security risks. As a result, healthcare providers have had to invest in secure EHR systems, encryption technologies, and robust cybersecurity measures to protect ePHI.
HIPAA's impact on healthcare technology extends beyond security. The act has encouraged the development of interoperable systems, allowing for the secure exchange of health information between different providers and systems. This interoperability has the potential to improve patient care, reduce errors, and enhance the overall efficiency of the healthcare system.
HIPAA and Patient Empowerment
HIPAA has also empowered patients by giving them greater control over their health information. The act grants patients the right to access their health records, make corrections, and receive a summary of disclosures. This transparency fosters trust between patients and healthcare providers, allowing individuals to actively participate in their healthcare decisions.
Furthermore, HIPAA's emphasis on patient consent and the limitations on the use and disclosure of PHI have given patients more agency over their personal health data. Patients can now make informed choices about how their information is shared, ensuring that their privacy is respected and their data is used ethically.
The Future of HIPAA: Evolving Challenges and Opportunities
As the healthcare landscape continues to evolve, so too must HIPAA and its regulations. The digital transformation of healthcare, the rise of telemedicine, and the increasing use of health apps and wearable devices present new challenges and opportunities for HIPAA compliance.
Addressing Emerging Technologies
With the proliferation of digital health technologies, HIPAA must adapt to address the unique security and privacy concerns associated with these innovations. The OCR has issued guidance on HIPAA compliance for mobile health apps and telemedicine, but ongoing efforts are needed to keep pace with technological advancements.
As more healthcare services move online, ensuring the security and confidentiality of patient data in the digital realm becomes crucial. This includes protecting patient information in cloud-based systems, securing data transmission during telemedicine consultations, and addressing the privacy risks associated with health tracking apps and wearable devices.
Interoperability and Data Sharing
The concept of interoperability is gaining momentum in healthcare, with the goal of creating a seamless flow of health information between different systems and providers. HIPAA supports this vision by encouraging the secure exchange of PHI, but challenges remain in achieving true interoperability while maintaining data privacy and security.
Standardizing data formats, implementing secure data exchange protocols, and ensuring that patient consent is respected during data sharing are critical aspects of achieving interoperability while adhering to HIPAA guidelines.
Data Analytics and Research
The vast amount of health data generated in the digital age presents opportunities for advanced analytics and research. However, using PHI for research and analytics purposes while maintaining patient privacy and confidentiality is a delicate balance. HIPAA allows for the use of de-identified data for research, but the process of de-identification must comply with rigorous standards to ensure patient anonymity.
As data analytics becomes increasingly important in healthcare, finding ways to leverage PHI for research and innovation while adhering to HIPAA guidelines will be a key challenge for the industry.
Conclusion
The Health Insurance Portability and Accountability Act of 1996 is a critical piece of legislation that has transformed the healthcare industry’s approach to patient data. By establishing national standards for the protection of PHI, HIPAA has empowered patients, improved the security of health information, and enhanced the efficiency of the healthcare system.
As the healthcare landscape continues to evolve, so too must HIPAA regulations. The act's ability to adapt to emerging technologies, support interoperability, and balance data analytics with patient privacy will be crucial in shaping the future of healthcare. Staying informed about HIPAA guidelines and best practices is essential for all stakeholders in the healthcare industry, ensuring that patient data remains protected and healthcare services continue to improve.
What is HIPAA and why is it important?
+HIPAA stands for Health Insurance Portability and Accountability Act. It is a federal law in the United States that sets national standards to protect sensitive patient health information from being disclosed without the patient’s consent or knowledge. HIPAA is important as it ensures the privacy and security of individuals’ health data, promotes efficiency in healthcare, and empowers patients to have control over their personal health information.
Who does HIPAA apply to?
+HIPAA applies to covered entities, which include healthcare providers, health plans, and healthcare clearinghouses. It also covers business associates of these entities who have access to protected health information (PHI). This includes a wide range of organizations and individuals involved in the provision, payment, and operations of healthcare services.
What are the key provisions of HIPAA?
+HIPAA consists of several key provisions, including the Privacy Rule, Security Rule, and Breach Notification Rule. The Privacy Rule establishes national standards for protecting PHI, while the Security Rule focuses on the protection of electronic PHI (ePHI). The Breach Notification Rule requires covered entities to notify individuals and the Department of Health and Human Services (HHS) in the event of a breach of unsecured PHI.
How can I ensure my organization is HIPAA compliant?
+Ensuring HIPAA compliance requires a comprehensive approach. Organizations should conduct regular risk assessments, implement robust security measures, and provide thorough training to their workforce. This includes adopting encryption technologies, access controls, and developing policies and procedures that align with HIPAA guidelines. Additionally, staying updated with the latest HIPAA regulations and seeking expert advice can help maintain compliance.