Health Insurance Businesses

Health insurance is a critical aspect of modern healthcare systems, playing a pivotal role in ensuring individuals have access to essential medical services. The health insurance industry is a complex and ever-evolving sector, with numerous players, intricate regulations, and a vast array of products and services. This comprehensive guide aims to delve into the world of health insurance businesses, shedding light on their operations, challenges, and future prospects.
Understanding the Health Insurance Landscape
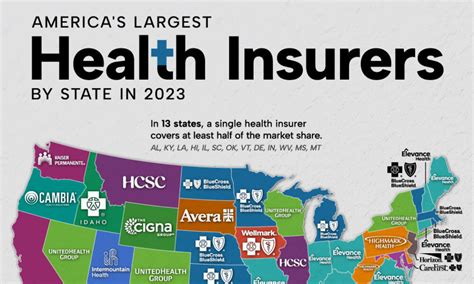
The health insurance industry is a multifaceted domain, encompassing a wide range of organizations, from large, multinational corporations to smaller, regional providers. These businesses operate within a highly regulated environment, governed by federal and state laws that dictate the terms of coverage, pricing, and consumer protections.
At its core, health insurance serves as a financial safeguard for individuals and families, providing coverage for medical expenses that could otherwise be financially devastating. By pooling resources from a large number of policyholders, insurance companies are able to offer comprehensive plans that cover a range of healthcare services, including doctor visits, hospital stays, prescription medications, and specialized treatments.
The health insurance market is primarily divided into two main segments: private and public. Private health insurance is typically purchased by individuals or provided by employers as a benefit. It offers a wide range of plan options, allowing consumers to choose coverage that best suits their needs and budgets. On the other hand, public health insurance, such as Medicare and Medicaid in the United States, is government-funded and caters to specific populations, such as seniors, low-income individuals, and those with disabilities.
Key Players and Market Dynamics
The health insurance industry is characterized by a diverse range of stakeholders, each playing a unique role in the healthcare ecosystem. Insurance companies, also known as carriers or providers, are the backbone of the industry. They design and administer insurance plans, negotiate rates with healthcare providers, and manage the financial risks associated with healthcare delivery.
Insurance carriers operate under various business models. Some are for-profit entities, driven by shareholder returns and focused on cost-efficiency. Others are not-for-profit organizations, often with a mission to provide affordable healthcare coverage to their communities. Additionally, there are health maintenance organizations (HMOs) and preferred provider organizations (PPOs), which operate under different network models and reimbursement structures.
Healthcare providers, including hospitals, clinics, and individual practitioners, are crucial partners in the health insurance ecosystem. They deliver medical services to insured individuals and negotiate contract terms with insurance companies to ensure fair reimbursement for their services. The negotiation process is complex, as it involves balancing the providers' financial needs with the insurance companies' cost management strategies.
Furthermore, the rise of technology has led to the emergence of new players in the health insurance space. Digital health startups and tech-savvy insurers are leveraging data analytics, artificial intelligence, and telemedicine to offer innovative solutions and enhance the efficiency of healthcare delivery. These players are disrupting traditional insurance models and driving the industry towards a more consumer-centric approach.
Challenges and Innovations in Health Insurance
Despite its critical role in healthcare, the health insurance industry faces several challenges that impact its operations and reputation.
Cost Containment and Affordability
One of the most significant challenges is the rising cost of healthcare and the subsequent impact on insurance premiums. The increasing complexity and cost of medical treatments, coupled with an aging population, put pressure on insurance companies to manage expenses effectively while maintaining adequate coverage for their policyholders.
To address this challenge, insurance companies employ various strategies, including negotiating lower rates with healthcare providers, implementing cost-sharing mechanisms such as deductibles and co-pays, and promoting preventive care to reduce the likelihood of costly illnesses. Additionally, the shift towards value-based care models, where providers are reimbursed based on patient outcomes rather than the volume of services delivered, is gaining traction as a potential solution to curb rising costs.
Regulatory Environment and Compliance
The health insurance industry operates within a highly regulated environment, with federal and state laws governing every aspect of insurance coverage, pricing, and consumer protections. Compliance with these regulations is essential to avoid legal repercussions and maintain public trust.
Key regulations in the health insurance sector include the Affordable Care Act (ACA) in the United States, which mandates essential health benefits and prohibits insurers from denying coverage or charging higher premiums based on pre-existing conditions. The ACA also established health insurance marketplaces, providing a platform for consumers to compare and purchase insurance plans.
Insurance companies must navigate these complex regulations, regularly updating their policies and practices to ensure compliance. This often requires significant investment in legal and compliance teams, as well as robust data management systems to track and report on various metrics, such as network adequacy and patient access to care.
Adopting Digital Transformation
The health insurance industry is undergoing a digital transformation, driven by the need for efficiency, improved customer experience, and cost reduction. However, this transformation presents its own set of challenges, as insurance companies must adapt to new technologies and digital trends while maintaining data security and privacy.
One of the key aspects of digital transformation in health insurance is the shift towards electronic health records (EHRs) and the integration of data analytics. By leveraging advanced analytics, insurance companies can identify patterns and trends in healthcare utilization, enabling them to make more informed decisions about coverage and pricing. Additionally, the use of digital platforms and mobile apps allows for real-time claim submissions and policy management, enhancing the overall customer experience.
Performance Analysis and Future Prospects
The health insurance industry's performance is closely tied to the broader healthcare sector and the overall economic climate. Over the past decade, the industry has experienced steady growth, driven by an aging population, increasing healthcare costs, and the expansion of health insurance coverage under the ACA.
According to a report by the Kaiser Family Foundation, the health insurance market in the United States is expected to reach $1.4 trillion by 2024, with a compound annual growth rate of 4.5%. This growth is attributed to the continued demand for healthcare services, the expansion of Medicaid coverage, and the increasing adoption of value-based care models.
| Year | Health Insurance Market Size (USD) | Compound Annual Growth Rate |
|---|---|---|
| 2020 | $1.1 trillion | 4.3% |
| 2021 | $1.2 trillion | 4.6% |
| 2022 | $1.3 trillion | 4.4% |
| 2023 | $1.35 trillion | 4.2% |
| 2024 (Projected) | $1.4 trillion | 4.5% |

However, the industry's future growth and prospects are not without challenges. The ongoing COVID-19 pandemic has highlighted the vulnerabilities of the healthcare system and the insurance industry, with insurers facing increased costs due to higher utilization of healthcare services and the impact on economic activity. Additionally, the industry must adapt to evolving consumer expectations, with a growing demand for personalized and flexible insurance plans.
Looking ahead, the health insurance industry is expected to continue its transformation, with a focus on innovation, digital integration, and consumer-centric models. The rise of telehealth services and the integration of artificial intelligence in claim processing and fraud detection are likely to become mainstream practices, enhancing efficiency and reducing costs. Furthermore, the industry will need to navigate the complex landscape of healthcare policy and regulatory changes, adapting to ensure the sustainability and accessibility of health insurance coverage for all.
Frequently Asked Questions

What are the different types of health insurance plans available?
+Health insurance plans come in various forms, including Preferred Provider Organizations (PPOs), Health Maintenance Organizations (HMOs), Point-of-Service (POS) plans, and High-Deductible Health Plans (HDHPs). PPOs offer flexibility with a broad network of providers, while HMOs typically require you to choose a primary care physician and refer you to specialists within their network. POS plans combine features of both PPOs and HMOs, and HDHPs have higher deductibles but often come with Health Savings Accounts (HSAs) for tax-advantaged savings.
How do health insurance premiums work?
+Premiums are the regular payments you make to your insurance provider to maintain coverage. The cost of premiums can vary based on several factors, such as your age, location, the type of plan you choose, and any additional benefits or coverage options you select. Premiums are typically paid monthly or annually.
What is the role of the Affordable Care Act (ACA) in the health insurance industry?
+The ACA, also known as Obamacare, was enacted to increase the quality and affordability of health insurance. It established health insurance marketplaces, mandated essential health benefits, and prohibited discrimination based on pre-existing conditions. The ACA also expanded Medicaid coverage and introduced tax credits to help make insurance more affordable for low- and middle-income individuals.
How does the health insurance industry ensure data privacy and security?
+The health insurance industry takes data privacy and security seriously, implementing various measures to protect sensitive information. This includes encrypting data during transmission and storage, employing access controls to limit who can view or modify data, and regularly conducting security audits and training to ensure compliance with privacy regulations like HIPAA.



